 Using local consensus on the definition of futile, Huynh et al have returned to suggest and quantify an ‘opportunity cost’ (i.e. a detriment to others due non-futile care) incurred.
Using local consensus on the definition of futile, Huynh et al have returned to suggest and quantify an ‘opportunity cost’ (i.e. a detriment to others due non-futile care) incurred.
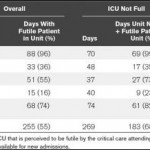
At a single centre, 5 unit hospital, delay in admission from A&E and delay in transfer to a tertiary ICU were examined and the impact of futile care on these delays assessed.
‘Futile’, ‘probably futile’ and non-futile treatment were not clearly defined and were subjective to the extent of depending on the specific coincidence of patient, doctor and hospital state of busyness. The same group has previously published on the same topic, finding that, in their single centre experience approximately 7% of hospital patient days were spent delivering costly futile care. 15% of those receiving futile care were still alive 6 months later but generally with a low quality of life. It is not clear in this week’s article how many patients were directly affected by delay in treatment, or to what detriment. In addition, figures from these studies will not be directly applicable to your institution, but the principles are intuitive and are likely to be transferable to some degree. It is surely no surprise that on less busy days there was a greater proportion of patients receiving futile treatment.
However, how often is it clear that treatment on the unit is futile in an absolute sense? Does the slippery term ‘futile’ really have a different definition for any given day/unit/doctor? Do we really operate a first-come-first-served system? The last chance to eke out what might be a tiny percentage chance to return to an acceptable life is often requested of intensivists. We know we are often a poor judge of the chance of success and also what an acceptable outcome is. Moreover, do some patients have a ‘better death’ on ICU, and if so is that of calculable value?
